By Anne Bodmer Lutz, M.D.
“And for all those tea drinkers out there: Let’s learn a lesson from tea. It shows it’s real worth when it gets into hot water” ~ Annonymous
“There are questions which illuminate, and there are those that destroy. We should ask the first kind” ~ Quote from Nobel physicist Isaac Isador Rabi.
Suicide presents a major challenge to public health in the United States and worldwide. Current global estimates indicate that approximately one million people die by Suicide each year, accounting for more than half of all violent deaths in the world. (Ting, Sarah, A., et al.). In the mental health field, managing “risk” is the dominant paradigm in responding to suicidal thoughts and behaviors. Risk assessment focuses on ensuring the client’s safety and minimizing the danger of harm without treatment. A solution-focused safety assessment (SFSA) is a paradigm shift providing an additive dimension to conventional risk assessment and cultivates hope. It highlights individual, and relationship resources (VIPs), coping strategies, reasons for living, and client needs. An SFSA emphasizes how clients have coped and managed to endure, even a little bit, the seemingly overwhelming distress that they have found unbearable at the moment.
INTRODUCTION TO SFSA
In my practice, I often am challenged with clients coping with suicidal thoughts and behaviors. Incorporating an SFSA has been very helpful both for my clients, their VIPs, and managing my own anxiety in these very stressful situations. Preparing clients for questions that evaluate their safety, by explaining that these questions are routinely asked, helps to normalize their struggles, aiding them in feeling less alone. Framing questions about safety in the context of “pain” and “good reason” imparts empathy. Asking clients their “good reasons” for behaviors that appear harmful (i.e.) self-harm, drug use, staying in a domestically violent relationship, to name a few, reveals how clients engage in these behaviors because in some way they are useful and beneficial for them. The question does not condone the behavior but instead helps to understand the client’s motivation and can help lead the conversation towards alternatives. When clients have contemplated suicide and not followed through, it is essential to ask what kept them from acting on their thoughts — asking clients their reasons for living guides the conversation towards their hopes, goals and future dreams.
Below is a picture of my Solution-Focused Safety Scale (SFSS)
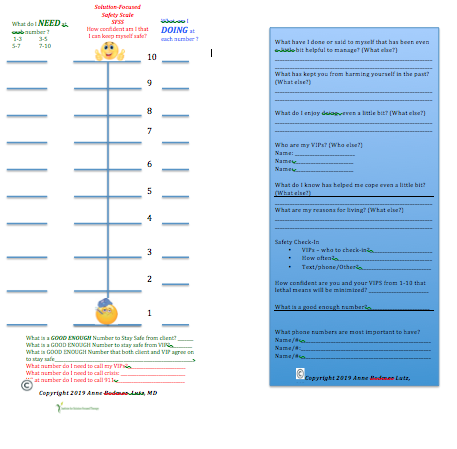
I keep a stack of solution-focused safety cards available in my office. I write the plan on the card with the client present and, if possible, also include their VIPs in the conversation. I have found the act of giving them the safety card which we have worked on together and which can be kept with them at all times, provides a tangible reminder of the work with have accomplished as a team. It can cue them to their strengths, resources, and coping strategies in times of distress.
SFSA and creating a “VIP Map.”
Inquiring about a client’s VIPs early on and throughout the conversation broadens “who” the client is and assists in integrating their unique social context within the dialog. VIPs highlight relationship resources, enhancing possibilities for solutions. Assessing who is a client’s VIPs is critical in understanding and assisting them in building solutions from the multiple perspectives of those most important in their life. VIPs are often the primary reason people stop themselves from acting on destructive thoughts. VIPs may include spouses, friends, children, teachers, coaches, grandchildren, pets, people whom they feel responsible for, and even people who may have died but whom they keep in their heart. Below are questions I ask to create a client’s “VIP map.”
- Who are the most important people in your life?
- Who else? Who else?
- What do you most appreciate about them?
- What else? What else?
- Who was “worried” or “concerned” about you that they thought coming here would be helpful for you?
- Do you have pets? How are they helpful for you? What do you most appreciate about them?
- Whose wellbeing do you feel responsible for?
- Who relies on you for help and support?
SFSA SCALING
On the front of the card is a picture of a scale from 1-10 (10 being the best). Solution-focused scaling questions are constructed in such a way that the 10 highlights a positive direction of where the clients want to go. When performing an SFSA, scaling questions measure how confident the client is that they can keep themselves safe. It is important to “work the scale.” Asking a variety of questions that amplify the scale often uncovers more opportunities to compliment clients and cultivate hope. Below is a list of questions that can “work the scale”.
What do you “KNOW” questions
- What do you know you need to do to keep yourself safe?
- This is asked to both clients and their VIPs
- What else do you know you need to keep yourself safe?
What have you “TRIED” questions
- What have you tried that has helped you endure these very painful moments and make them “even a little bit tolerable?”
- What else have you found has helped you cope to make it even a little bit bearable for you?
- What would your VIPs say has helped you manage these moments in a bearable way? What else would they say?
Scaling CONFIDENCE in safety: “On a scale from 1-10, where ten is the best:”
- How confident are you that you can keep yourself safe?
- What keeps the number from being lower?
- What else keeps it from being lower?
- What would be a “good enough” number?
- What would you be doing at this “good enough” number?
- What else would you be doing?
- What would your VIPs notice you are doing at this “good enough number?
- What else would your VIPs notice you doing?
- How would you discover when it goes up by one point?
- What would you be doing? What else would you be doing?
- How confident would you predict your VIPs would say you can keep yourself safe?
- What was the highest number it has been?
- When was this?
- What were you doing at that number? What else were you doing?
- What do you think helped the number be higher at those times? What else helped?
- At what number would you require a higher level of care, such as going to the emergency room, calling 911, or calling a crisis team?
- At what number would your VIPS say you require a higher level of care?
- How confident are you from 1-10 that you can do the necessary things you need to keep yourself safe?
Scaling a “Good enough” number to keep safe
Scaling can also help clients and their VIPs confirm what they need at particular numbers. Of particular importance is to confirm a “good enough number” in which they know they can keep themselves safe. This is important to ask both to clients and confirm with their VIPs. If clients think they can keep themselves safe and their VIPs do not agree, it is critical to detail the reasons for the discrepancy. What is the reason the client is confident 10/10 they will keep themselves safe, but their VIP thinks it is only a 2? Ensuring a client can maintain their safety requires confirmation that their VIPs are in agreement.
Asking clients what number they would be at if things are “not good enough” and they do not feel confident in their ability to keep themselves safe affords an opportunity to detail what they would be doing at that number and connecting that number to what they need. When things are “not good enough”, they may report behaviors such as contemplating Suicide, staying in their room for much of the day, not talking, sleeping all day or not have the energy to do what is required of them. Detailing the actions of clients at each of the numbers and correlating these actions to what they need acknowledges their pain while elucidating to both clients and their VIPs a concrete plan of action that corresponds to their needs. They may need to call someone, have someone stay with them, go for a walk, pet their dog, call a crisis hotline, or go to the emergency room. What is critical is to refrain from assuming what you think they need, and instead ask both clients and their VIPS what they know is required at each particular number. I have found this level of detail reassuring to clients and their VIPs, as well as equipping them with a highly individualized plan that can be mutually confirmed.
Safety Number Check-Ins with VIPs
Scaling questions also limit language confusion and assist in creating a safety plan that both the client and their VIPs can agree on. Asking clients if they think it would be helpful to have someone do a “safety number check- in” provides a way for clients and their VIPs to assess confidence in their safety quickly and easily. Inquiring with clients who they think would be most helpful to check in with, how often, and by what method (i.e.) text, phone, email, can incorporate their VIPs within a safety plan in tangible ways.
Indirect Compliments and Positive Differences
Clients and their loved ones are understandably very distressed when suicide is disclosed. Providing indirect compliments to clients in the form of a question (How did you do it?) invites clients to appreciate what they have already done and are doing to cope with their painful situation. The meticulous use of past tense verbs highlights that clients have already done something to cope with their painful situation and thus can do it again. How did they decide to have the courage to ask for help? How have they endured their pain, even if only a little bit? How have they managed even if for brief times to keep from acting on the suicidal thoughts? These moments may seem negligible and can be easily passed over in a clinical encounter, yet it is these seemingly “micro-positive” differences that are critical to amplify in times of despair. What clients are doing to cope in seemingly small ways are the very things they need to do more of to endure their situation. These positive differences may include when clients were able to get through part of a day, got dressed, talked or texted a friend, cared for their pet, ate some food, drank a cup of tea, helped a friend, accomplished even a small part of a goal, and stopped themselves from acting on their suicidal thoughts. Amplifying these differences by exploring whether these differences were helpful, how they are helpful and how they accomplished these differences uncovers additional resources.
Highlighting situations as temporary instead of permanent
“Rewording,” a client’s “permanent language” to “temporary” can help clients endure their situation even “a little bit.” Emphasizing the temporary nature of their situation can subtly impart hope. For example, when a client says “I don’t see any way out,” rephrasing it to “right now,” it doesn’t feel like there is a way out. Or when clients say nothing seems to matter, rewording their statement to “It seems right now” nothing seems to matter.
A Language of Empathy: “For You” Statements
Clients and families who are struggling with suicide often experience hopelessness, fear, anger, and anxiety, requiring a great deal of “for you” responses. Examples of “For You” statements with clients might be acknowledging how exhausting it must be “for you” to endure the suffering and painful situation you have been dealing with. For parents and loved ones, it might be validating how scary and frightening it must be “for you” to see your child struggling with suicide. Acknowledging how difficult it must be “for them” confirms their emotional perspective and can help them tolerate their situation even a little bit.
SFSA Risk Assessment
An SFSA integrates solution-focused language in a “traditional” risk assessment. The following are SFSA risk assessment questions.
- How well from 1-10 (10 being the best) are you managing your mood, anxiety, cravings, substance use, and other health conditions? What are good enough numbers for these domains? What do they need to help them manage these areas?
- Have you ever had to cope with domestic violence, abuse, natural disasters, war, homelessness, substance use, loss, divorce?
- How have you coped? How else?
- Have you ever had to cope with prior suicidal ideation or behaviors?
- How did you cope?
- What kept you from acting on those thoughts? What else?
- What treatments/providers/medications have been most helpful for you?
- What do know has been most helpful about your prior treatments/ providers and medications?
- How satisfied are you from 1-10 with your most important relationships?
- Has anyone in their family had to cope with depression, substance use, suicide, or other mental health conditions?
- What do you know has been helpful for them?
- Who in your family is doing well?
- What do you know about what has helped your family members who are doing well?
- How well from 1-10 are you managing your work and financial stress?
- What is a good enough number? What keeps the number from being lower?
- How satisfied are you from 1-10 with the treatment and resources available to you in your community?
- Do you have guns/ unlocked medications in your home?
- What do you know is needed to manage these means of harm? How confident from 1-10 are you that you can do what is needed to minimize these lethal means?
- What is a good enough number?How confident from 1-10 are your VIPs that the lethal means can be minimized in the home can be minimized?
- How confident are you that you can call and ask for help if you are not feeling confident in your safety?
- Whose phone numbers are most important for you to have? Who else?
Remaining solution-focused when a higher level of care is needed
When a client requires a higher level of care, it is still possible to stay solution-focused. The following questions can help to sustain a solution-focused conversation encouraging both patients and their VIPs to be involved in this difficult decision while conferring a sense of control and responsibility.
- What are the patient’s best hopes for hospitalization?
- What are their VIP’s best hopes for their hospitalization?
- How are they hoping the hospitalization will be helpful?
- What will tell them they are ready to leave the hospital and have learned the necessary skills to keep safe?
- What will tell the client’s VIPs that they have learned the necessary skills to help their loved one stay safe?
Resources if you are need of help now
The National Suicide Prevention Lifeline number is: 1-800-273-8255
For the National Text Hotline, text the word TALK to 741741
Locally, the crisis line for Call2Talk is 508-532-2255. Or text C2T to 741741
The American Foundation for Suicide Prevention has additional resources at https://afsp.org/find-support/
REFERENCES
Castro, Sahily De, and Jeffrey T. Guterman. “Solution-Focused Therapy for Families Coping with Suicide.” Journal of Marital and Family Therapy, vol. 34, no. 1, 2008, pp. 93–106., doi:10.1111/j.1752-0606.2008.00055.x.
Fiske, Heather. Hope in Action: Solution-Focused Conversations about Suicide. Routledge, 2008.
Henden, John. Preventing Suicide: the Solution Focused Approach. Wiley, 2017.
Kondrat, David C, and Barbra Teater. “Solution-Focused Therapy in an Emergency Room Setting: Increasing Hope in Persons Presenting with Suicidal Ideation.” Journal of Social Work, vol. 12, no. 1, 2010, pp. 3–15., doi:10.1177/1468017310379756.
Lutz, Anne Bodmer. Learning Solution-Focused Therapy: an Illustrated Guide. American Psychiatric Publ., 2014.
Ronquillo, Linda, et al. “Literature-Based Recommendations for Suicide Assessment in the Emergency Department: A Review.” The Journal of Emergency Medicine, vol. 43, no. 5, 2012, pp. 836–842., doi:10.1016/j.jemermed.2012.08.015.
“The Solution Focused Approach in Working with the Suicidal.” Preventing Suicide, 2017, pp. 123–151., doi:10.1002/9781119162926.ch8.
Ting, Sarah A., et al. “Trends in US Emergency Department Visits for Attempted Suicide and Self-Inflicted Injury, 1993–2008.” General Hospital Psychiatry, vol. 34, no. 5, 2012, pp. 557–565., doi:10.1016/j.genhosppsych.2012.03.020.
